Children's Blocked Nose
Children's Blocked Nose (Adenoids, Allergy in Children, mouth breathing) can be a problem of:
Disturbed sleep (Sleep Disordered Breathing)
A child’s blocked nose may contribute to disturbed sleep in the form of restlessness during sleep, poor sleep quality, tiredness during the day. Recent sleep disordered breathing research suggests that disturbed sleep can significant impacts on school performance, reduced blood levels of oxygen and occasionally can affect blood pressure and heart performance.
Facial Growth
With long standing nasal blockage a child’s mid-face may not grow as well as the other parts of their face. This changes the appearance of the child (in medical terms a version of this is called Adenoid Facies). The upper jaw can change in shape and contribute to a high arch palate and crowding of teeth.
Exercise impairment
With a blocked nose a child sometimes struggles with physical activity due to the restriction of airflow. Swimming can be a struggle and sports on grass if the child has a component of allergic rhinitis (hayfever) can be particularly distressing.
Speech Impairment
A blocked nose can produce a nasally type of speech (medically this is called a “hyponasal” voice). This can make it difficult for the child to be understood. Large, bulky adenoids (which sit behind the palate) can stop the palate from moving freely and contribute to this “hyponasal” voice.
Poor Teeth
Dental research shows that with long standing mouth breathing there is an increased risk of dental caries, discoloured teeth (from enamel dehydration) and poor alignment of teeth (with a higher chance of requiring orthodontics). Treatment of mouth breathing and a blocked nose in a child is suggested before secondary (adult) teeth erupt, which commonly starts at the age of 6 to 7.
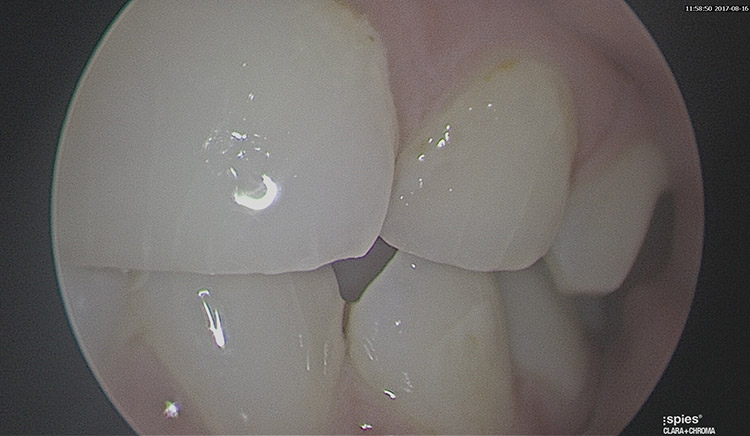
Above: Poor teeth from mouth breathing – demonstrating vertical fracture lines and erosion of the enamel from teeth grinding.
A/ Prof Nirmal Patel
MBBS (Hons), FRACS (OHNS) MS (Research UNSW)
Specialising in Endoscopic Ear Surgery for Cholesteatoma and Chronic Ear Infection, Eustachian Tube Surgery, Cochlear Implant and Lateral Skull Base Surgery. Other interests are Children’s ENT disorders.
Dr Leo Pang
BSc (Med) MB BS FRACS (OHNS)
Specialising in Adults’ and Children’s Ear, Nose and Throat disorders, with a subspecialty interest in Head and Neck Cancer Surgery, Salivary Gland Surgery, Thyroid Surgery.
Dr Justin Kong
MBBS Bsc (MED) MMed FRACS (ORL-HNS)
Specialising in Endoscopic Sinus and Nasal Airway Surgery as well as Anterior Skull Base Surgery. Other interests are Children’s Ear, Nose and Throat disorders.
Dr Fiona Ting
MBBS (Hons 1) BSc (Med) MClinEpid, FRACS (OHNS)
Specialising in Endoscopic Sinus and Nasal Airway Surgery as well as Anterior Skull Base Surgery. Other interests are Children’s Ear, Nose and Throat disorders.
Videos relating to Children's Blocked Nose
What are the common causes of a blocked nose in children?
Adenoid tissue is located at the back of the nose, above the palate. The purpose of the tissue is to help the body develop immunity in the first few years of life. The adenoid tissue can grow to block the nose. If the child is symptomatic then surgery to remove the adenoids is offered. Adenoidectomy is day surgery procedure performed under a full general anaesthetic with a camera through the nose and instruments through the mouth. Usually the child is sore for 1 to 2 days and off school for 2 days.
The nose lining can get inflamed for various reasons most commonly from either allergy or viral infection (colds and flus). Allergic nose swelling in the nose is common in children (up to 40% of children will have form of allergic symptoms). When the allergy is longstanding the normal side cushions of the nose (called turbinates) swell and can block the nose. Initial treatment for a blocked nose includes saline and nasal steroid spray. Allergy management including allergy avoidance and immunotherapy may be useful. Surgery to reduce the size of the turbinates including either turbinate cautery or turbinoplasty (used in older children) is used if the medical measures do not work.
The bone and cartilage in the midline of the nose divides it into right and left. The division is called the nasal septum. In a small percentage of children as their nose grows the bone and/or cartilage can twist and block the nose. Another common cause of deviated septum in children is following a broken nose. Generally unless the child is struggling with sleep and diagnosed with obstructive sleep apnoea, the deviated septum is not fixed until the age of around 16 when the nose has stopped growing. This is because surgery on the septum when the child is growing can affect the external nose shape.
Many other rarer causes are present for blocked noses in children including a lack of formation of the nose airway on one side (unilateral choanal atresia), cysts (antrochoanal polyp), congenital birth defects (dermoids, encephaloceles) and other rare conditions.
Your ENT Surgeon will assess the causes of your child’s blocked nose and offer the appropriate treatment option.
Other Services
Other Services
Still have a question?
Our team will be happy to answer any questions you may have about Children’s blocked noses.